HPV-vaccination
Prevo-Check®-test, Munic
Prevo-Check® - blood test in Munich - an innovative tumor marker test for the early detection of HP virus-related, sexually transmitted cancers in the genital and oral pharyngeal region of men and women.
In times of increasing globalization and growing carelessness during sexual intercourse with changing partners, sexually transmitted infections and precancerous lesions have been on the rise again worldwide and thus also in Germany for several years.
Along with genital herpes and chlamydia, genital warts are one of the most common sexually transmitted infections (STI).
Also known as genital warts, condylomata accuminata or condylomas, these brownish red nodules in the genital and anal areas, usually the size of a pinhead, are caused by the human papilloma virus (HPV).
Human papilloma viruses (HPV) are transmitted to the human intimate or oropharyngeal area mainly through unprotected sexual intercourse, infected semen, and, rarely, also through shared towels or bathing with infected persons.
In men, sexually transmitted warts usually develop in the area of the penis shaft, foreskin, urethra or in the anal and rectal area. In women, they usually occur on the labia, vaginal entrance, anus, rectum or cervix.
Mother-to-child transmission is also possible during birth and can lead to warts in the genital area of the newborn, and rarely also to condylomas in the throat.
On the basis of the different genetic material, a distinction has been made to date between more than 100 different HP virus subtypes, whereby HP virus types 6 and 11 usually cause benign genital warts only weeks or months after the actual infection in 90 percent of cases.
To diagnose genital warts, the treating urologist or gynecologist will first examine the external genital and anal region more closely as part of a physical examination. If the urologist finds genital warts in the external genital or anal region of the male or female patient during the physical inspection, it is recommended that the man undergoes further rectoscopy or meatoscopy, because genital warts in men can also spread unnoticed in the rectum and/or urethra.
In women, the gynecologist also examines the cervix with the aid of a colposcope (special microscope), with which the skin surface of the cervix can be shown in detail, and greatly enlarged optically.
Treatment
The treatment of genital warts can be done with special solutions (Podophyllotoxin) or creams (Imiquimod, Interferon) or they can be removed by icing, electro-resection or laser therapy (see laser therapy).
Due to the fact that there is currently no treatment method that can guarantee complete elimination of the papilloma virus (HPV) and therefore no complete cure, urologists and gynecologists advise that patients suffering from genital warts should undergo regular check-ups following treatment.
Biopsy
Before any condyloma treatment, a tissue sample should be taken from the wart tissue in order to be able to perform an HPV subtype analysis in a specialist pathology laboratory, because the potentially high-risk virus types 16, 18 and 31 found there are held responsible for the development of penile cancer in men and for the development of cervical cancer in women.
If a high-risk HPV infection of type 16, 18 or 31 with or without the development of genital warts does not heal completely, the virus-infected cells can develop into precancerous lesions in the cervix - and in the anal area in women, in the penis - and in the anal area in men over time.
Through annual cancer screening, these precancerous lesions can be detected and their early treatment can prevent the development of cancer.
Until now, the early detection of cervical cancer in women has mostly been carried out by means of the so-called PAP test, in which mucous membrane cells are removed from the region of the cervix using a cotton swab and examined under the microscope for suspicious changes.
However, HPV-related cancers do not only affect the urogenital tract. As a result of oral sex or smear infections, these viruses can also cause cancer of the mucous membrane (squamous cell carcinoma) in the mouth and throat.
Rapid test in Munich
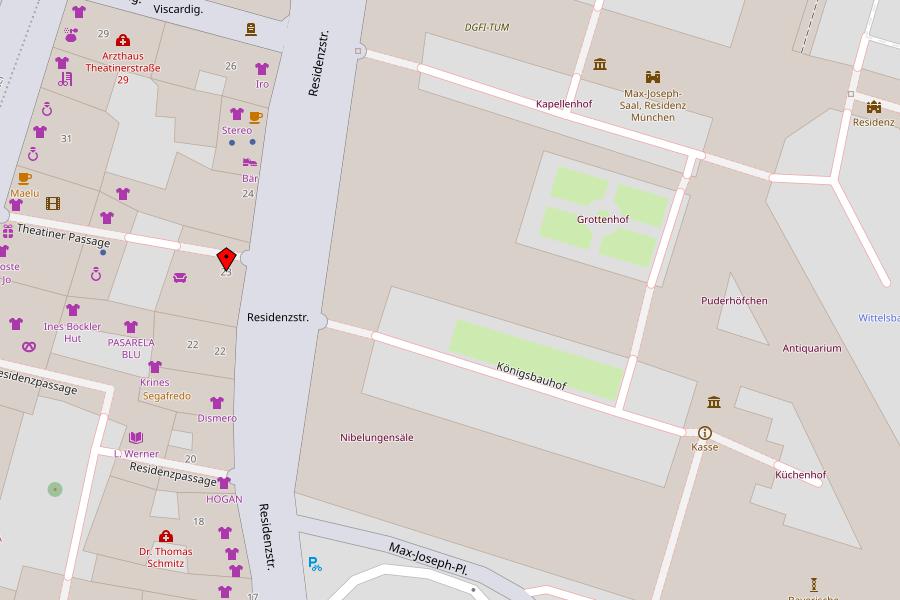
Our private urological practice in Munich offers you the Prevo-Check® , a new, innovative rapid test for the early detection of HPV-related cancer (carcinoma) in the genital and oral pharyngeal area.
For the examination, a drop of blood is obtained through a tiny puncture from the earlobe or fingertip.
The rapid test detects highly specific serum antibodies against HPV16 in this drop of blood, which are directly related to the presence of the cancer precursors explained above.
Depending on the situation, you will receive the result from us within a few minutes or during your next visit to our practice.
The test has a specificity of almost 100 percent and thus shows almost no false positive results.
This means that patients who test positive should be examined by the urologist and gynecologist for HPV-related carcinomas of the urogenital tract and in any case be referred to an ENT specialist to rule out precancerous lesions or carcinomas.
The Prevo-Check® can be carried out easily and quickly and offers you as a patient more safety through diagnostics that conform to guidelines.
Early detection allows for gentle treatment options as well as a significantly improved prognosis.
(If cancer-suspicious mucosal lesions can already be visually detected in a patient, a cell smear or brush biopsy should also be performed in order to be able to initiate further DNA analyses for virus typing).
Examinations for the early detection of diseases are basically aimed at apparently healthy and symptom-free persons.
Screening is designed to detect a disease or its precursor before it causes symptoms."
Source: Federal Ministry of Health
HPV vaccination: for consideration
In the meantime, there is also a vaccination against human papilloma viruses, which protects against the two most common pathogens - virus types 16 and 18 - in particular.
This can effectively prevent precancerous lesions and thus cancer of the cervix caused by the two types of HPV.
Since infection with HPV can already occur during the first sexual contact, it seems sensible to vaccinate adolescents before their initial sexual activity.
The permanent vaccination commission at the Robert Koch Institute (STIKO) has therefore recommended that all girls between the ages of 9 and 14 (but no later than their 18th birthday) should generally be vaccinated against human papillomavirus types 16 and 18.
However, because not all sexual intercourse is necessarily accompanied by an HPV infection, vaccination still seems to make sense even after the first sexual intercourse.
In boys, vaccination is recommended from the age of 9 because vaccination stimulates the production of antibodies against HP viruses and can thus prevent the development of genital warts, depending on the vaccine.
The guidelines for physicians on the prevention of HPV-associated tumors also recommend vaccination from the age of 9.
It can be assumed that uninfected children and adolescents who are nowadays vaccinated against HPV 16 before having sexual intercourse for the first time will not develop HPV16-related cancers of the genital and pharyngeal regions many years later.
![[Translate to Englisch:] Logo Urologische Privatpraxis Dr. med. Friedemann Meisse](/fileadmin/_processed_/2/f/csm_urologe_muenchen_ec59653cb9.png)
![[Translate to Englisch:] prevo-check-HPV-viren dr. meisse muenchen [Translate to Englisch:] prevo-check-HPV-Viren](/typo3conf/ext/min_interchange/Resources/Public/Images/invis.gif)