TULA® laser therapy for genital warts
State-of-the-art laser technology for the effective and lasting treatment of condylomas (genital warts) in Munich
Genital warts, also known as condylomas, condylomatous warts or genital warts, are a sexually transmitted infection (STI) caused by certain types of the human papillomavirus (HPV). These warts occur in the genital area, including the penis (foreskin, penis shaft, glans), vulva, vaginal canal, labia, anus and surrounding skin. They can also occur in the mouth and throat, especially during oral sex.
Genital warts (condylomata accuminata) are "cauliflower-like" painless skin tumors that can vary in size, shape and color. They can occur singly or in groups and can be flat or raised. In some cases they cause no symptoms, while in others they cause itching, pain, burning or bleeding.
As the human papillomavirus (HP virus) is highly contagious in the condyloma stage, we recommend effective laser therapy at our private urology practice in Munich. This is particularly advisable if previous medical treatments with ointments or cautery solutions (such as imiquimod/podophyllotoxin) have not been successful.
Genital warts should always be treated. Although they are harmless in most cases, they can trigger precancerous stages or cancer in certain risk variants of the human papillomavirus.

State-of-the-art laser therapy
In our practice, we carry out genital wart laser therapy using the state-of-the-art TULA® laser. Virus particles (virus DNA) can settle in the genital skin cells in the long term, this is also referred to as virus persistence. For this reason, genital condylomas tend to have a high reproduction and recurrence rate. Close follow-up by the urologist is therefore important, especially in the first few months after treatment. This applies to both pharmacological therapies and laser therapy.
How can genital warts (condylomas) be treated generally?
Genital warts can be treated in different ways - for example with creams (imiquimod) that stimulate the immune system to fight the virus or solutions (podophyllotoxin) that cause the warts to die, or by icing with nitrogen (cryotherapy). There are also other treatment options, however:
Laser therapy is currently considered the most effective treatment option for condyloma disease. Laser energy is used to denature (coagulate) and vaporize the condyloma.
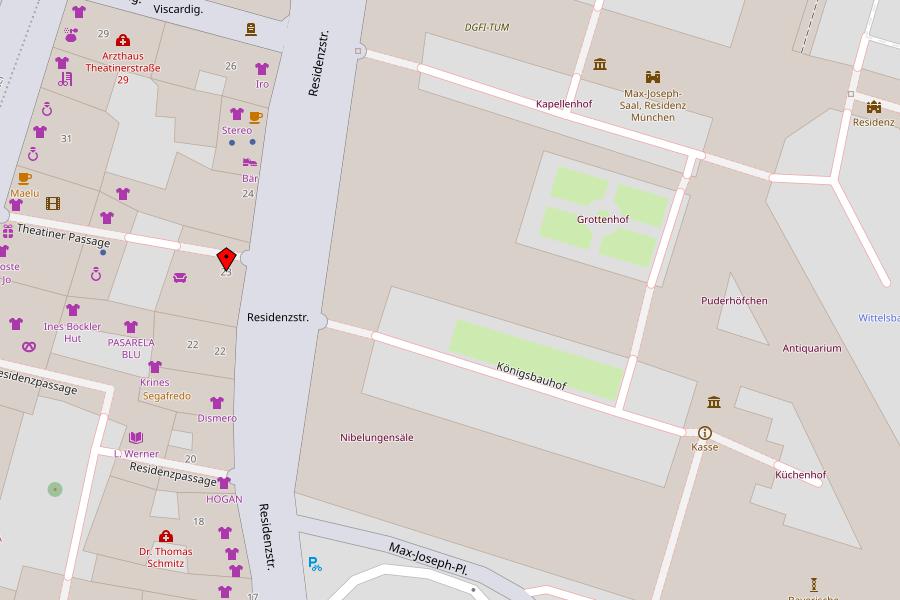
In contrast to surgical removal with a scalpel or electrocautery, the laser is gentle on the tissue, which means that scarring only occurs in very rare cases. With the ultra-modern TULA® laser system, the Urology Department at the Residence has a very effective laser system for the treatment of genital warts.
Advantages of TULA® laser therapy for the treatment of genital warts:
- Gentle on tissue
- No or minimal scarring (compared to scalpel surgery)
- Minimally invasive (without invasive bodily treatment)
- Can be performed on an outpatient basis
- Can be performed under local anesthesia
General information about genital warts:
What are genital warts (condylomata accuminata)?
Genital warts, also known technically as condylomata acuminata or genital warts, are a type of wart caused by certain strains of the human papillomavirus (HPV) - in particular by papilloma viruses of the risk group HPV 6 and 11 (low risk type) and HPV 16 and 18 (high risk type). To date, more than 140 different human papilloma viruses (= HP viruses) have been identified. The papilloma viruses are highly resistant and can be transmitted via fingers or inanimate vectors. Genital warts are small cauliflower-like, painless skin tumors. They occur in varying sizes and numbers and predominantly in the genital region (foreskin, penis shaft, glans and sulcus coronarius (ring-shaped depression behind the glans), vaginal canal, introitus vaginae (vaginal vestibule), labia). Condylomas are usually benign skin tumors. However, if left untreated for a long time, they can cause malignant skin cancer.
Are genital warts dangerous and should they always be treated?
Individual virus particles, i.e. the DNA of the virus, can settle in neighboring skin epithelial cells. The persistence of viral DNA in neighboring skin regions is responsible for the high recurrence rate of condylomas. The immune system is responsible for the eradication (complete removal of a pathogen) of the infection. This in turn means that a weakened immune system can make you more susceptible to HPV infection. An infection with certain so-called high-risk HPV viruses can cause precancerous lesions on the penis, in the cervix or in the mouth and throat (after oral sex). HPV DNA is detectable in precancerous lesions in almost 100 percent of cases and in invasive (growing into tissue) penile carcinomas in 50 percent of all cases.
Type 16 of the HPV virus in particular frequently causes invasive carcinomas, while types 18, 31, and 33 also occur more frequently. Infection with human papillomaviruses initially leads to the activation of viral oncogenes (genes that are activated by mutation and support the development of tumors). Oncogenes stimulate the production of so-called oncoproteins, which in turn block the breakdown of cancer-inhibiting cell substances in healthy skin cells. As a result, a healthy skin cell can mutate into a cancer cell (carcinoma cell). A reciprocal transfer of the cancer risk depending on the HPV infection from the woman to the man and vice versa is possible and scientifically proven. Genital warts should always be treated. Appropriate treatment can help to remove the warts, reduce the risk of passing them on to others and prevent possible complications.
Diagnosis of genital warts/condylomas/genital warts
- Careful inspection of the external genitals, groin and perianal region (area around the anus)
- with acetic acid improves the identification of small and flat genital warts (gray-white discoloration) after an appropriate period of exposure
- If the outer urethral orifice is affected, a cystoscopy is advisable, as genital warts can also grow inside the urethra and can therefore be easily overlooked during a simple inspection
Treatment options for genital warts/condylomas/genital warts
- Etching therapy with podophyllotoxin: 0.3 - 0.5 percent solution, twice daily for three days, then four days break from therapy, four cycles
- Immunotherapy with imiquimod: 5% cream applied three times a week for 16 weeks.
- TULA laser therapy: the most effective and sustainable form of therapy
Aftercare
- Close follow-up care for all treatment options
Prevention
To minimize the risk of HPV contamination and infection and to be able to assess the disease, we recommend
- Early education in families and schools about the risks of STIs (sexually transmitted infections)
- Condom/femidom use
- Reducing promiscuity, i.e. avoiding sexual intercourse with frequently changing partners, especially in the absence of condom use
- Vaccinations: Vaccinations against HPV are recommended for all young people between the ages of 9 and 14. Ideally, the vaccination should be given before the first sexual contact. Repeat vaccination is possible. HPV vaccines provide almost 100 percent protection against infection with the HPV types contained in the vaccines. Women and men who are 18 years or older can also benefit from HPV vaccination in individual cases, depending on their individual lifestyle
- Thorough physical examination of the genital region
- Laboratory diagnostics for suspected condyloma disease using PCR diagnostics (see PCR diagnostics in the urology department at the Residence)
- Histological examination of genital warts including typing for risk group affiliation
![[Translate to Englisch:] Logo Urologische Privatpraxis Dr. med. Friedemann Meisse](/fileadmin/_processed_/2/f/csm_urologe_muenchen_ec59653cb9.png)