Tissue-saving interventions
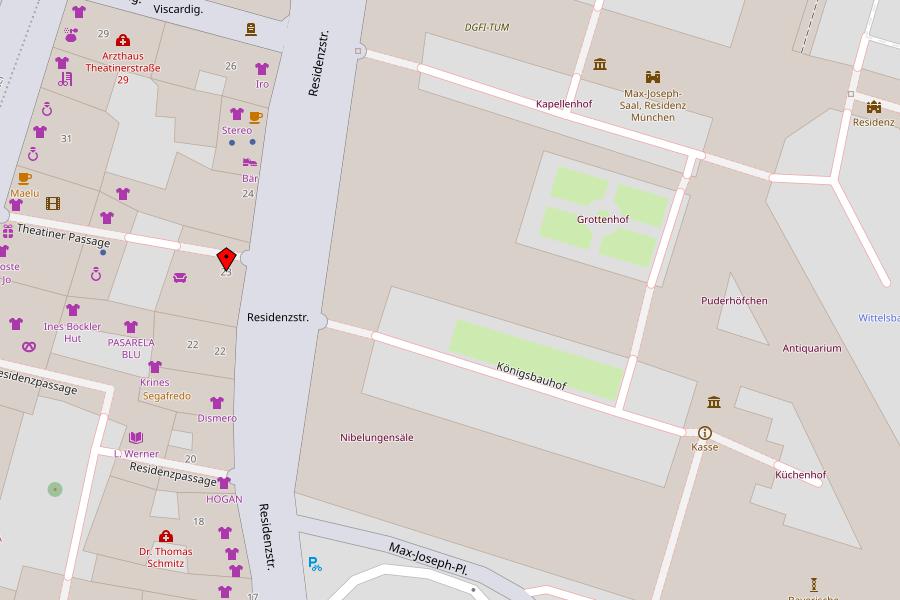
Urological laser therapies, Munich
Laser therapies are treatments that use lasers. The term laser stands for "light amplification by stimulated emission of radiation", which can be translated as "light amplification by stimulated emission of radiation". In this process, light with different wavelengths is strongly focused in different ways.
Lasers have become indispensable in medicine, as they can be applied very selectively and in the smallest of spaces, depending on the wavelength and power density of the laser radiation. Appropriate lasers such as neodymium YAG, holmium YAG, krypton, aron or CO2 lasers are available for different types of tissue. They have a tissue-ablating, tissue-destroying and also tissue-vaporizing effect.
The advantages of laser therapy are a very targeted, selective application with the greatest possible protection of the tissue, less bleeding and shortened healing time.
We use laser therapy in Munich for the treatment of:
- Genital warts
- Bladder tumors
- Urethral stenosis (narrowing of the urethra)
- Ureteral stenosis (narrowing of the ureter)
Sexually transmitted diseases on the rise
More and more people in Germany are becoming infected with sexually transmitted diseases, wrote Focus in November 2023. While "safer sex" was in vogue in the 1980s with the increased occurrence of the HIV/AIDS virus, it seems to have fallen out of focus today. The Focus article points out that the number of cases of syphilis alone has tenfold in the last 20 years. While there were around 800 syphilis infections in 2000, today there are around 8,300. There has also been a similar increase in other sexually transmitted diseases (STDs): According to the Robert Koch Institute, the number of people infected with hepatitis B, for example, rose from 3,875 in 2001 to 15,990 in 2022, an almost five-fold increase. In addition, there would be around 300,000 new chlamydia infections every year and there would also be a rapid increase in gonorrhea, hepatitis C and herpes and human papilloma viruses (HPV). The Focus also writes: Around 60 percent of diagnosed throat cancers are due to HPV, as they are also transmitted via oral sex. (Source Focus online, Thursday, Nov. 9, 2023)
Advantages of our PCR analyzer for the detection of sexually transmitted infections (STIs)
- Painful sampling by means of a smear from the urethra is generally no longer necessary because urine is used as the sample material.
- It is no longer necessary to send samples to a large-scale laboratory, which saves valuable diagnostic time.
- The analysis result is available to us after two and a half hours; in contrast to the large-scale laboratory, where the result is usually only evaluated after three days.
- Any necessary (antibiotic) therapy can therefore be started promptly.
- Rapid partner diagnostics and partner therapy possible; in the event of a positive test result, your partner can also be tested by us for an STI. In the event of STI contamination by the partner, appropriate treatment can then be started at the same time.
Which STI pathogens can we detect with our PCR analyzer?
- Chlamydia trachomatis (chlamydia)
- Neisseria gonorrhoeae (gonorrhea)
- Trichomonas vaginalis (trichomonas)
- Treponema pallidum (syphilis/lues)
- Herpes simplex virus I (virus)
- Herpes Simplex Virus II (virus)
- Mycoplasma hominis (bacterium)
- Mycoplasma genitalium (bacterium)
- Ureaplasma urealyticum (bacterium)
- Haemophilus ducreyi (bacterium)
Due to their dangerous nature, syphilis, hepatitis B and AIDS must be reported in Germany in accordance with the Infection Protection Act (IFSG) in order to limit their spread.
HIV (AIDS) and hepatitis B can only be diagnosed by a blood test, HPV only by a urethral swab. To clarify these pathogens, we send the blood samples and the swab to a large-scale laboratory.
What is a PCR test, such as the one we carry out in our practice in Munich?
PCR tests have become indispensable in modern medicine and molecular diagnostics. Due to its high precision, PCR, which stands for polymerase chain reaction, is now considered the "gold standard". This is a biochemical method for the amplification of certain DNA sequences.
The principle of PCR measurement is based on two steps: In the first step, the genetic material of a germ/pathogen, known as DNA, is amplified. Even the smallest traces of a pathogen are sufficient to detect it. In the second step, the genetic material is sorted and characterized in order to analyze its origin. In other words, the affiliation of the DNA is determined, which enables the pathogen (virus/bacteria) to be precisely identified.
Read general information about sexually transmitted diseases here
What are sexually transmitted infections (STIs) in general?
In principle, anyone can come into contact with a sexually transmitted infection (STI) in the course of their life. Some STI pathogens can lead to unpleasant urogenital infections but are essentially harmless. Others, however, can even be life-threatening.
Sexually transmitted infections that are detected early can usually be easily treated, although not all of them are (yet) completely curable. Sexually transmitted diseases can be caused by various pathogens. Syphilis, gonorrhea and chlamydia infections, for example, are caused by bacteria. STIs such as HIV (human immunodeficiency virus), hepatitis B virus (HBV), herpes labialis and genitalis as well as human papillomas (condylomas/prickly warts), on the other hand, are caused by viruses. Fungi (candida) and parasites (e.g. trichomonads) can also cause sexually transmitted diseases.
The risk of transmission varies depending on the pathogen and the site of infection (vaginal, anal, oral). For example, the risk of contracting HIV through oral sex is low. It is possible to contract several sexually transmitted infections at the same time. Sexually transmitted infections are mainly transmitted during sexual intercourse (vaginal, anal, oral). With some pathogens (e.g. fungi, chlamydia), smear infection is possible. A sexually transmitted infection can also be passed from the mother to her child during pregnancy, childbirth or breastfeeding. Some sexually transmitted infections can be transmitted through direct blood contact, for example by sharing injecting equipment during drug use.
What are the typical symptoms of sexually transmitted diseases?
The symptoms of a sexually transmitted infection can be just as varied as the pathogens themselves. It is therefore advisable for patients to always consult a specialist (urologist/gynecologist) if they suspect they have contracted a sexually transmitted infection. It is not uncommon for there to be no symptoms at all.
The following symptoms/discomforts may indicate an STI:
- Burning sensation when urinating
- Noticeable foul-smelling discharge from the vagina, anus or penis/urethra
- Itching, pain or skin changes in the genital area (vagina, anus)
- Pain in the genital area, bladder or lower abdomen
- Painful sexual intercourse
- Changes in the mouth and throat or rectum after oral or anal intercourse
- Tiredness, fatigue, fever, loss of appetite, sore throat
How do sexually transmitted infections progress and how can they be treated?
Many sexually transmitted infections can be cured if treatment is started early and consistently. It is also important that the sexual partner is also examined if an STI is suspected and treated if necessary. Although some sexually transmitted infections, such as HIV/AIDS, cannot be cured, their health consequences can often be controlled with ongoing treatment. HPV infections cannot be cured by treatment either, but most HPV infections heal on their own within one to two years. The Urology Department at the Residence also offers vaccination for particularly relevant HPV types. Vaccination can prevent persistent (ongoing) infections and possible secondary diseases.
If treatment is delayed or not received, various complications or late effects can occur, which can vary in severity depending on the infection. The pathogens can spread throughout the body and infect other organs. Without treatment, HIV continuously damages the immune system so that other pathogens become increasingly difficult - and eventually impossible - to fight off.
A syphilis infection goes through several stages if left untreated. If syphilis pathogens have infected the central nervous system, late damage can occur in the form of paralysis and sensory disorders, but they can also cause permanent damage to other organs. If left untreated, the gonorrhea pathogen can cause inflammation of the joints, eyes and heart, as well as permanent infertility. If gonorrhea pathogens pass from an infected pregnant woman to the child during birth, the newborn can go blind. The risk of premature birth is also statistically increased in the case of untreated gonorrhea or trichomonas infection.
Genital chlamydia infection can lead to unwanted sterility, pregnancy complications and infections in newborns. Human papillomaviruses (HPV) can cause cancer of the cervix, vagina, vulva, mouth/throat, anus, and penis if the infection persists. HP viruses are also responsible for genital warts (condylomata accuminata). Although these warts are harmless, they are highly contagious and perceived as a cosmetic and psychological burden, not least because of their stigmatizing appearance.
We can treat genital warts in a tissue-friendly, effective and cosmetically clean way with the TULA® laser on an outpatient basis under local anesthesia in our practice. Numerous risk types are known from the family of HPV viruses - whereby the high-risk HPV types are responsible for almost all precancerous stages/cancer development in the cervix. Chronic hepatitis B infection can lead to liver cirrhosis (liver scarring) and malignant liver tumors (liver cell cancer).
How can you protect yourself from sexually transmitted infections?
There is a wide variety of protective measures. Listed below are the most important ones:
- Early education in families and schools on the risks of STIs
- Condom/femidom use (but does not offer 100% protection) - The aim is to avoid the exchange of potentially infectious bodily fluids (safer sex). These include, for example, blood (menstruation), semen and vaginal fluids. These fluids can contain pathogens and can be transmitted through contact with mucous membranes.
- Promiscuity reduction, i.e. avoiding sexual intercourse with frequently changing partners, especially in the absence of condom use.
- Vaccinations against individual pathogens (e.g. hepatitis B virus and HPV) and pre-exposure prophylaxis if there is an increased risk of HIV infection are currently available. Vaccinations against HPV are recommended for all young people between the ages of 9 and 14. Ideally, the vaccination should be given before the first sexual contact. Repeat vaccination is possible. HPV vaccines provide almost 100% protection against infection with the HPV types contained in the vaccines. Men and women who are 18 years or older can also benefit from HPV vaccination in individual cases, depending on their individual lifestyle. Basic immunization against hepatitis B usually takes place within the first 11 months of a child’s life. If this has not been done, basic immunization is recommended for adolescents between the ages of 9 and 17. In adulthood, the Standing Committee on Vaccination (STIKO) recommends vaccination against the hepatitis B virus for certain indications, such as certain professions.
For some years now, there has been an effective protection option for HIV, known as HIV pre-exposure prophylaxis (PrEP). This medication issuitable for HIV-negative people who have an increased risk of contracting HIV. There is also post-exposure prophylaxis (PEP). This involves taking HIV medication for four weeks promptly after a risk contact to prevent infection. Today's HIV drugs are very effective. With regular and successful therapy, they prevent HIV from multiplying in the body and therefore not only protect the health of HIV-positive people, but also prevent transmission during sexual intercourse. This is known as "protection through therapy". Effective therapy for HIV-positive pregnant women also prevents HIV transmission to the child. Timely clarification of an STI when the first symptoms appear (PCR diagnostics in the urology department at the Residence) - for example, detecting and treating a sexually transmitted infection as early as possible during pregnancy examinations reduces or prevents the transmission of germs from mother to child.
![[Translate to Englisch:] Logo Urologische Privatpraxis Dr. med. Friedemann Meisse](/fileadmin/_processed_/2/f/csm_urologe_muenchen_ec59653cb9.png)