TULA® laser therapy for bladder cancer
State-of-the-art laser technology for the gentle treatment of bladder cancer in Munich
Dr. Meisse is one of the first urologists in southern Germany to use the minimally invasive, safe TULA® laser procedure to treat bladder cancer in their practice. In addition, Dr. Meisse is currently one of the first urologists in Germany to offer TULA® laser treatment in combination with photodynamic diagnostics (PDD) in flexible endoscopy in his practice.
Photodynamic diagnostics (PDD) is also a state-of-the-art procedure that is otherwise only used in clinics for the diagnosis and clarification of bladder tumors. PDD works with fluorescent light, which makes flat-growing, usually aggressive bladder tumors in particular visible at a stage where this is not possible with conventional methods. Find out more about photodynamic diagnostics (PDD) here.
The advantages of TULA® laser therapy for bladder cancer/bladder tumors:
- Minimally invasive procedure = surgery using small incisions in the skin (no open surgery)
- Precise removal of the tumor; therefore tissue-sparing procedure = healthy tissue is spared
- Outpatient implementation Very low risk of infection (infections can be virtually ruled out)
- particularly painless
- NO general anesthesia
- Short treatment time (the laser procedure itself takes around 30 minutes)
- Quick return to usual activities possible Minimal and only minor side effects, therefore also suitable for older people and patients at risk
What is TULA® laser therapy?
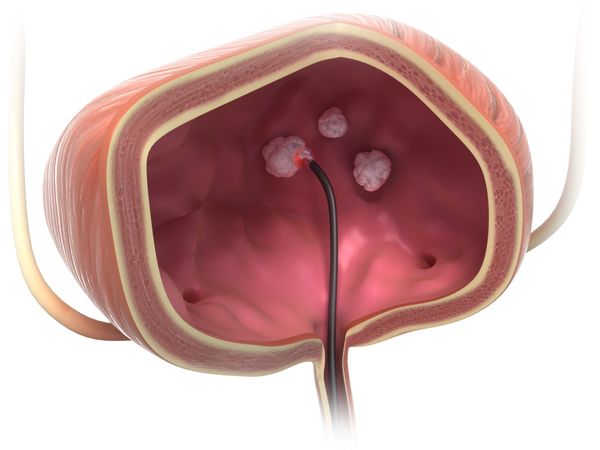
TULA stands for transurethral laser ablation. It is an ultra-modern, effective and yet gentle treatment method that can be used to treat bladder tumors endoscopically using laser energy. This applies in particular to well-differentiated, superficial bladder tumors that have not yet grown into the bladder muscle.
Dr. Meisse - whose private urological practice is based in Munich - is one of the few urologists in private practice in southern Germany who use this minimally invasive laser therapy for bladder cancer treatment in their practice.
Urinary bladder cancer - two categories
Urinary bladder cancer/bladder tumors are malignant cancers of the urinary bladder. Bladder cancer can essentially be divided into two categories, depending on how deeply the cancer cells have grown into the bladder lining. In around 75 percent of cases, the initial diagnosis of bladder cancer is a so-called "non-muscle-invasive bladder cancer" (NMIBC) - in other words, a stage in which the tumor remains limited to the superficial layers of the mucous membrane and has not grown into the bladder muscle. This stage of cancer is considered an early tumor stage with a relatively good prognosis. A bladder tumor at this stage can be successfully treated with a high cure rate by endoscopic removal of the tumor (for example with laser therapy).
In contrast to so-called "muscle-invasive bladder cancer" (MIBC), where the entire bladder usually has to be surgically removed. Superficially growing bladder tumors have a significantly better healing and therefore survival rate than tumors that have already grown into the bladder muscle. In addition, the bladder can usually be preserved in the case of non-muscle-invasive bladder cancer. Preserving the organ means a significantly better quality of life, as artificial urinary diversion or the creation of a so-called "neobladder" from intestinal tissue is not necessary.
TULA® laser therapy - as used by Dr. Meisse in his private practice at the Urology Department at the Residence in Munich - is particularly suitable for non-muscle-invasive bladder tumors. This minimally invasive, gentle laser treatment method usually leaves the bladder intact.

How is TULA® laser therapy carried out?
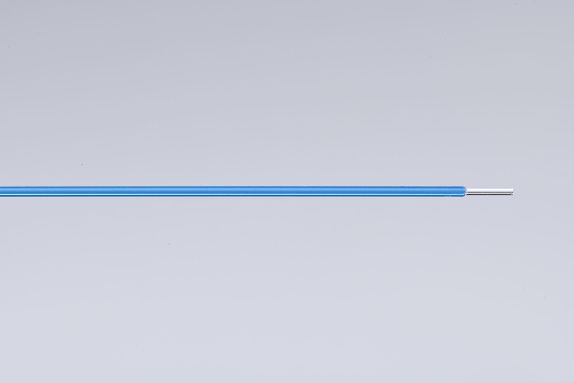
TULA® laser therapy/laser treatment is performed on an outpatient basis in Dr. Meisse's practice in Munich city center or in an outpatient surgery center such as the IATROS Clinic. With the help of a flexible endoscope - also known as a cystoscope - the bladder is first scanned and the tumor visually identified. The endoscope is a tubular, three to four millimeters thick, flexible optic with an integrated camera system. Using this endoscope, an extremely thin laser fiber is advanced to the tumor in a controlled manner via a screen and the tumor is completely destroyed with laser energy (= intensive light energy) through vaporization and tissue denaturation (coagulation).
Photodynamic diagnostics (PDD) and TULA® laser therapy in combination - bladder cancer diagnostics and therapy from a single source
Dr. Friedemann Meisse in Munich is currently the only urologist in private practice in Germany who can offer flexible TULA® laser endoscopy in combination with photodynamic diagnostics (PDD). PDD has a high additional benefit in the early and recurrent detection of bladder cancer. A recurrence in this context is a recurrence of a tumor disease. The simultaneous use of PDD and TULA® enables optimal early tumor detection combined with maximum gentle tumor removal, both of which are important for reducing the recurrence rate.
What other technical advantages does TULA® laser therapy offer?
Another advantage of the TULA® laser procedure is that the intense laser energy can be used to "seal" the surrounding and tumor-carrying vessels so that any blood supply to the tumor and the adjacent tumor regions is cut off. In contrast to the conventional TURB procedure, this "vascular sealing" significantly and effectively prevents tumor cells from flowing into the bloodstream with the risk of tumor cell seeding in other regions of the body (= metastasis). The risk of local tumor cell seeding, i.e. tumor cell spread within the urinary bladder, is also minimized by laser-induced vascular obliteration compared to the resection procedure (TURB). Because TULA® therapy, unlike conventional "transurethral resection TURB", does not require the tumor tissue to be cut out of the bladder wall, the risk of injuring or even perforating the bladder is minimal, not least due to the fact that the TULA® laser penetration depth in the tissue is focused and very shallow.
What other advantages does TULA® laser therapy, as we perform it in our urology practice in Munich, offer patients?
- Outpatient implementation
- NO special preparation necessary as with procedures under general anesthesia (patient can eat as usual on the day of the procedure)
- Can be performed under local anesthesia (on request, we can also perform the treatment under a gentle sleep anesthesia (sedoanalgesia) or general anesthesia on an outpatient basis)
- Minimally invasive laser procedure with virtually no risk of bladder wall injury (perforation) in contrast to conventional transurethral tumor resection (TURB)
- Protection of the surrounding mucosal tissue
- For patients with comorbidities and for whom general anesthesia is no longer possible, applicable patients who need to take "blood thinners" due to cardiac diseases need not discontinue these for pending TULA® treatment
- Recurrent general anesthesia can be avoided. In terms of tumor genetics, superficial bladder carcinomas have an increased recurrence rate (recurrence of the disease). With conventional treatment methods, this means multiple general anesthetics, which in turn is associated with increased risks (especially memory impairment in older patients). With the TULA® procedure, no recurring general anesthesia is required.

Patient information for download
Download a patient information leaflet (PDF) by clicking the image:
Learn more about bladder cancer causes/risk factors/symptoms
What is the difference between a cancer cell and a normal cell?
Growth: Normal, healthy body cells stop growing and multiplying when there are enough cells and a cell defect (e.g. a wound) has been repaired (= orderly cell division). Cancer cells, on the other hand, divide and grow unchecked, stimulated by uncontrollably produced oncoproteins (growth factors). This results in a cluster of cells (tumor).
Communication: Normal cells communicate with their neighboring cells and stop growing when they come into contact with them. Cancer cells do not do this, they grow "unchecked".
Cell repair and cell death: Normal cells are either repaired or die (apoptosis = natural, ordered cell death) when they are damaged or become old. Cancer cells are not repaired and do not undergo orderly cell death (apoptosis).
Localization: Normal cells adhere to each other in the cell network with the help of protein bridges (adhesion molecules) and remain at the site of their formation. Cancer cells do not do this. They can "float away", i.e. spread throughout the body and form new cell clusters (tumors) elsewhere in the body, which are also known as metastases.
The urinary bladder is the organ in which the urine produced by the kidneys over a 24-hour period is stored. When the bladder is full, we feel the urge to urinate and typically empty the stored urine when convenient via the urethra. Bladder cancer is a malignant tumor (carcinoma) and originates from the uppermost mucous membrane layer of the bladder, the so-called urothelium. This is why we also refer to bladder cancer as urothelial carcinoma or urinary bladder carcinoma. As the urothelium lines the entire urinary tract, it can also occur in the renal pelvis, the ureters and also in parts of the urethra. In almost 90 percent of cases, however, urothelial carcinoma develops in the bladder. Around 30,000 people are diagnosed with bladder cancer in Germany every year, over 70 percent of whom are men. Bladder cancer is usually a cancer of older patients over the age of 65, but this does not mean that bladder cancer cannot occur at a much earlier age (!).
Bladder cancer is currently the fourth most common tumor disease in men and the twelfth most common in women.
Risk factors for the development of bladder cancer are:
- Smoking is the most common cause of bladder cancer. Smokers have a threefold higher risk of bladder cancer. 50 percent of all bladder cancers are diagnosed in smokers. Certain toxins (so-called aromatic amines/naphthylamines) from inhaled tobacco smoke enter the urinary bladder via urinary excretion from the kidneys. These amines damage the urothelial cells, thus preventing controlled (physiological) cell division of the bladder epithelial layer and cancer develops as a result of "unchecked" cell growth.
- Occupations that come into increased contact with aromatic amines, such as chemical workers, employees in the steel and leather processing industry and in the rubber industry, car mechanics, roofers, but also dental technicians and hairdressers have an increased risk of developing bladder cancer/urothelial carcinoma.
- Radiation/medications: People who have undergone radiotherapy due to another cancer or people who are/were exposed to increased radiation (for example, the Chernobyl nuclear disaster in 1986) have/had a statistically increased risk of developing bladder cancer in the longer term, depending on the region of the body in which the radiation dose is/was highest. The drug cyclophosphamide (Endoxan), a cytostatic drug used to treat certain cancers and autoimmune diseases, also has a statistically increased risk of developing bladder cancer.
- There may also be a familial predisposition to the development of bladder cancer if parents or siblings have already developed bladder cancer.
- Infectious disease: In tropical and subtropical countries (for example in Egypt), urinary bladder carcinoma can occur as a late consequence of schistosomiasis (tropical infectious disease). This disease is caused by a parasite (sucker worm) living in fresh water, which enters the human organism through the skin, spreads as a host via the bloodstream and can settle in the human urinary bladder wall. Within the bladder wall, this parasite can cause bladder cancer.
- Urinary bladder emptying disorders/difficult urination/prostate enlargement: Urological diseases that permanently disrupt bladder emptying, such as benign or malignant prostate enlargement (prostate adenoma/prostate carcinoma), urethral stricture or neurological (nervous) muscle weakness of the bladder (contraction insufficiency) increase the risk of incomplete bladder emptying. This results in residual urine, i.e. the contact time between urine and urothelium in the bladder is prolonged and toxins in the urine that are due for excretion (e.g. aromatic amines) have a longer toxic effect on the urothelium with the risk of carcinoma formation.
Symptoms of bladder cancer – what are the signs of bladder cancer?
In the early stages, bladder cancer usually causes little or no symptoms. The most common symptoms include
- Blood in the urine: The painless appearance of blood in the urine (painless hematuria) can be a first warning sign. This can be detected microscopically (microhematuria) or even with the naked eye (macrohematuria).
- Frequent urge to urinate: Bladder cancer can lead to an increased urge to urinate, especially in combination with bladder inflammation (cystitis) or urinary bladder emptying disorders.
- Painful urination: Bladder cancer can cause pain when urinating, just like bladder inflammation
- Bone pain: Since, as described above, bladder cancer cells can lead to cell metastases in the bone, especially in advanced tumor stages, these can cause bone pain, particularly in the spine (back pain) or in other bone regions.
- Respiratory disorders/liver dysfunction: Soft tissue metastasis, i.e. spread of bladder cancer cells to the lungs or liver, can lead to respiratory disorders/chest pain or liver dysfunction (e.g. jaundice).
![[Translate to Englisch:] Logo Urologische Privatpraxis Dr. med. Friedemann Meisse](/fileadmin/_processed_/2/f/csm_urologe_muenchen_ec59653cb9.png)